Strategic Leadership and Future Delivery Models. 1
HCAHPS Scores for Intermountain Medical Center 1
HCAHPS scores for Intermountain Hospital 2
HCAHPS scores for Intermountain Medical Center Hospital 3
Mean calculation for each of the Nurse’s Top-Box: 3
Nurse communication composite mean (Y) score: 3
Analysis of the HCAHPS Scores. 3
Comparison of HCAHPS Scores to State and National Averages. 4
Organizational Changer at Intermountain Medical Center in Comparison with Two Other Hospitals 5
How Educational Dynamics Could Potentially Influence HCAHPS Scores. 12
Short-Term and Long-Term Financial Impact 13
Causes of the Hospital’s HCAHPS Scores. 14
Organizational Strategic Plan. 15
Significance of Organizational Change. 15
How Organizational Change Can Help Improve the Chosen Hospital’s HCAHPS Scores. 16
The Quality Strategic Framework. 16
Structure, Process, and Outcomes of the Strategic Plan. 19
Incorporation of Evidence-Based Practice (EBP) and Shared Governance. 20
Incorporation of Technology. 22
Improving Care Delivery System.. 23
Methods of Improving the Care Delivery System.. 24
Improve Financial Stability. 24
Methods That Would Be Used to Improve Financial Stability. 25
Implementation Plan and Timeline. 25
Roles and Responsibilities of Stakeholders. 25
Key Roles and Responsibilities of Stakeholders. 26
Stakeholder Accountability and Involvement 26
How To Ensure Stakeholder Accountability And Involvement 27
Evaluation of the Strategic Plan. 29
Communication of Evaluation Results. 30
Strategic Leadership and Future Delivery Models
Healthcare is an integral pillar in the development of an economy. A country with a high health index tends to record better workforce performance, and this explains why there has been a significant focus on the improvement of the quality and reliability of the American healthcare sector (Grustam et al., 2020). As the demand for quality, affordable, and reliable medical care increases in the country, hospitals are restructuring their operational models to meet emerging needs. According to Cox and Amin (2020), the coronavirus pandemic has put immense pressure on the performance of the healthcare industry. The authors assert that hospitals with enhanced operational structures and facilities are better equipped to meet the needs of their clients. A cross-sectional survey conducted in 2013 found that hospital utilization is a major challenge in many countries in the world – equitable utilization of medical care is a challenge (Grustam et al., 2020). Like many other hospitals in the country, Intermountain Medical Center, holds the view that engaging patients in their personal choices leads to improved outcomes – improved care and enhanced patient satisfaction. While the hospital has satisfactory results based on its Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) star ratings, some segments need improvement. Hence, the focus of this business plan is to evaluate the current Intermountain Medical Center’s operations and performance and develop recommendations that will facilitate the improvement of its areas of weakness while leveraging the strengths.
HCAHPS Scores for Intermountain Medical Center
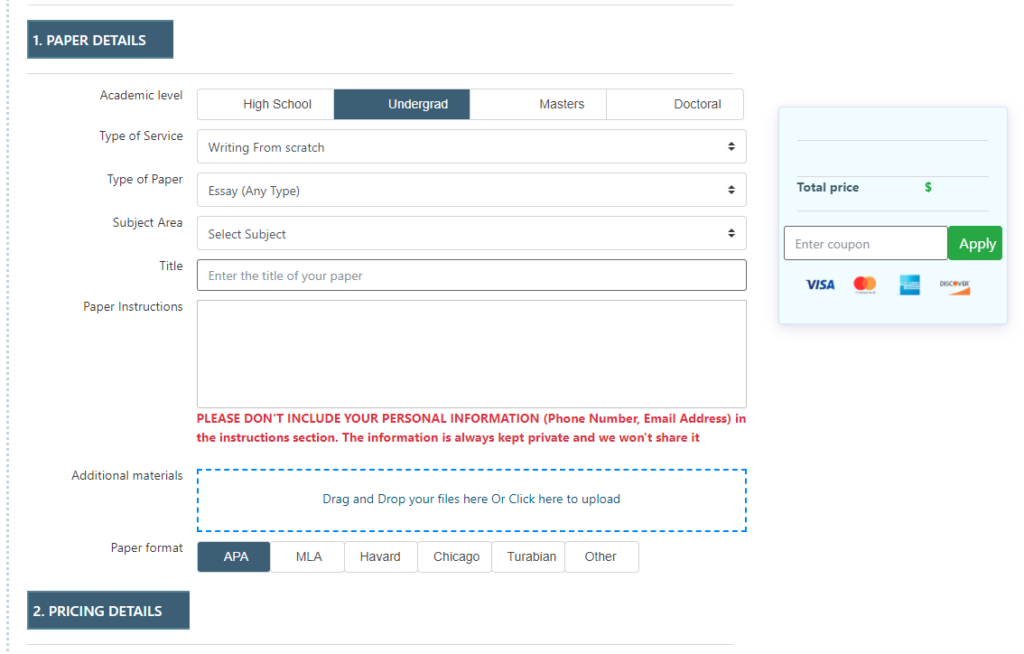
Intermountain Medical Center’s mission statement reflects its commitment and dedication to improving prevention and wellness in society. The organization strives to improve the health of the people in the community – ensuring that people live healthiest lives. At the same time, the hospital seeks to become a model of extraordinary care and superior service provision at an affordable cost to all people (Intermountain Healthcare, 2021). As depicted on its website, Intermountain Medical Center’s mission, vision, and values closely mirror its HCAHPS star ratings. Below is a description of Intermountain Medical Center’s HCAHPS survey, which not only illustrate the quality of care, but also the level of patient satisfaction compared to the national and Utah averages. See Image 1 below.
HCAHPS Scores for Intermountain Hospital
Image 1: HCHPS Survey (Medicare, 2020, c).
HCAHPS Scores for Intermountain Medical Center Hospital
Above is the survey that was completed at Intermountain Medical Center hospital. The HCAHPS scores were as follows in Table 1 below:
Table 1: HCAHPS Scores
| Survey Number | Q1 Response | Nurse 1 Top-Box | Q2 Response | Nurse 2 Top-Box | Q3 Response | Nurse 3 Top-Box |
| 1 | Always | 1 | Always | 1 | Sometimes | 0 |
| 2 | Always | 0 | Usually | 0 | Always | 1 |
| 3 | Sometimes | 1 | Sometimes | 1 | Always | 1 |
| 4 | Sometimes | 1 | Never | 0 | Always | 1 |
Mean calculation for each of the Nurse’s Top-Box:
Nurse 1 Top-Box mean = (1+0+1+1)/4 = ¾
Nurse 2 Top-Box mean = (1+0+1+0)/4 = 2/4
Nurse 3 Top-Box mean = (0+1+1+1)/4 = ¾
Nurse communication composite mean (Y) score:
Y = (Nurse 1 Top-Box mean + Nurse 2 Top-Box mean Nurse + 3 Top-Box mean) / 3 = ¾ + 2/4 + ¾) /3 = 6
Analysis of the HCAHPS Scores
With reference to nurse communication Top-Box, “Always” was the most positive response category for all the four questions that entail nurse engagement, activity and communication, as seen in Table 1 above. In other words, the response rate for the “Always” was high across the provided options during the survey (Medicare, 2020, c).
Comparison of HCAHPS Scores to State and National Averages
HCAHPS is the first national, standardized, publicly-reported survey of patients’ perspectives of hospital care. The HCAHPS Survey is a 29-item instrument and data collection methodology for measuring patients’ perceptions of their hospital experience. One of the most crucial significance of HCAHPS is that it allows valid comparisons to be made across hospitals — locally, regionally and nationally. The survey was nationally implemented in 2006 and public reporting of hospital scores began in 2008. Since 2012, HCAHPS scores have played a role in hospital payment through the Hospital Value-Based Purchasing program.
In terms of the overall rating, Intermountain (five stars) has the highest score, with the other two having four stars (University of Utah Hospitals and Clinics and St Mark’s Hospital). Patient survey rating differentiates the three hospitals. The HCAHPS scores show the University of Utah Hospital has the best patient experiences for medical care (four stars), followed by Intermountain Medical Center (three stars), and the least is St. Marks Hospital (two stars) (Medicare, 2020, a-c). The scores demonstrate that when it comes to patient experiences to medical care, Intermountain is an intermediate performer; hence, management needs to adopt strategies to enhance the impact of medical care and improve client experiences.
Apart from St. Marks Hospital, the University of Utah Hospitals and Clinics, and Intermountain have effective preventive care strategies since their scores are above the national average. However, the two organizations (Intermountain and University of Utah Hospitals and Clinics) struggle when it comes to cancer care, as their scores are below the national average. Pregnancy care and delivery is a matter that ought to be addressed in Intermountain. While the other two institutions of care have 0% of mothers being admitted too early than scheduled, Intermountain has 3% early schedules, above the national and Utah average.
Timely and effective care is an integral factor in the provision of medical care. Hospitals that can provide timely and effective care reduce the rate of readmissions, deaths, and complications. An evaluation of the three hospitals HCAHPs scores shows that the three hospitals have varying performance indexes. St. Marks Hospital has the best sepsis care (58%), followed by University of Utah Hospitals and Clinics (48%), and the least score is recorded by Intermountain (42%). The common factor between these hospitals is that their scores are below the national average (60%) and Utah average (62%) (Medicare, 2020, a-c). The scores demonstrate that more needs to be done to boost performance in the industry.
Organizational Changer at Intermountain Medical Center in Comparison with Two Other Hospitals
Intermountain Medical Center seeks to introduce a new structure to ensure better service to the patients and the community at large. For example, instead of its present time geographically demarcated administrative areas, the institution is generating a new system-wide design with two main groups, namely a Specialty Care Group and a Community Care Group (Medicare, 2020, c).
Accordingly, the Community Care Group is expected to take care of the patients through prevention and outstanding essential care, for example, fortifying and guaranteeing that patients get the medical examination and attention they should have, as well as assisting them control incurable illness like hypertension and ensuring they get outpatient treatment for comparatively insignificant medical needs (Medicare, 2020, c). On the other hand, the Specialty Care Group will deal with the inpatient care, and administering the care the patients need in the right way and the right time.
In other words, the organizational change at Intermountain Medical Center focuses mostly on how the patient exploit healthcare services and mirrors new communication platforms and structures that enable swift and more personal contact amongst patients, nurses and the hospital management. The new changes are expected to foster more value for the patient that seek treatment at Intermountain Medical Center. Prominently, the new changes are part of the ongoing innovation at Intermountain Medical Center. Compared to other facilities, this is a bold move that is expected to culminate into a more consistently pre-eminently patient encounters, whether at the hospitals or not. This change will assist the hospital to carry on providing the greatest quality care even at the lowest viable cost.
Comparison of Rate (Intermountain Medical Center to University of Utah Hospital and Clinic and St. Marks Hospital)
The HCAHPS Survey captures the patient’s experience of communication with doctors and nurses, responsiveness of hospital staff, communication about medicines, cleanliness and quietness of the hospital, discharge information, transition to post-hospital care and overall rating of the hospital. The survey is administered between 2 and 42 days after discharge to a random sample of adult patients. There are four approved modes of administration: Mail, Telephone, Mixed (mail with telephone follow-up), and Interactive Voice Response.
The performance of Intermountain Medical Center is compared against that of University of Utah Hospitals and Clinics and St Mark’s Hospital. While closely related, these three institutions exhibit some differences in terms of their performance and quality of care. The three healthcare institutions are rated as acute care hospitals that provide emergency care services and able to receive lab results electronically (Medicare, 2020, a-c). In terms of the overall rating, Intermountain (five stars) has the highest score, with the other two having four stars (University of Utah Hospitals and Clinics and St Mark’s Hospital). Patient survey rating differentiates the three hospitals. The HCAHPS scores show the University of Utah Hospital has the best patient experiences for medical care (four stars), followed by Intermountain Medical Center (three stars), and the least is St. Marks Hospital (two stars) (Medicare, 2020, a-c). The scores demonstrate that when it comes to patient experiences to medical care, Intermountain is an intermediate performer; hence, management needs to adopt strategies to enhance the impact of medical care and improve client experiences.
The HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey is the first national, standardized, publicly reported survey of patients’ perspectives of hospital care. HCAHPS (pronounced “H-caps”), also known as the CAHPS Hospital Survey, is a survey instrument and data collection methodology for measuring patients’ perceptions of their hospital experience. While many hospitals have collected information on patient satisfaction for their own internal use, until HCAHPS there was no national standard for collecting and publicly reporting information about patient experience of care that allowed valid comparisons to be made across hospitals locally, regionally and nationally.
Three broad goals have shaped HCAHPS. First, the survey is designed to produce data about patients’ perspectives of care that allow objective and meaningful comparisons of hospitals on topics that are important to consumers. Second, public reporting of the survey results creates new incentives for hospitals to improve quality of care. Third, public reporting serves to enhance accountability in health care by increasing transparency of the quality of hospital care provided in return for the public investment. With these goals in mind, the Centers for Medicare & Medicaid Services (CMS) and the HCAHPS Project Team have taken substantial steps to assure that the survey is credible, useful, and practical.
The HCAHPS survey asks discharged patients 29 questions about their recent hospital stay. The survey contains 19 core questions about critical aspects of patients’ hospital experiences (communication with nurses and doctors, the responsiveness of hospital staff, the cleanliness and quietness of the hospital environment, communication about medicines, discharge information, overall rating of hospital, and would they recommend the hospital). The survey also includes three items to direct patients to relevant questions, five items to adjust for the mix of patients across hospitals, and two items that support Congressionally-mandated reports.
The HCAHPS survey also collects basic patient demographics from five additional survey questions, including self-reported health status. CMS utilizes the demographic information and additional administrative data from hospital records to calculate and apply a patient mix adjustment (PMA) to each hospital’s score prior to publication. CMS states that “the goal of adjusting for patient mix is to estimate how different hospitals would be rated if they all provided care to comparable groups of patients.” The self-reported health status is a key variable in the patient mix adjustment that CMS applies to the scores. The HCAHPS process does not require reporting of additional patient clinical variables or other administrative data such as billing codes that could be used to strengthen the patient mix adjustment.
Intermountain Medical Center has the best colonoscopy follow-up, and it is above the national and Utah averages (98% – recommendations on time; 96% – patients with polyps receiving follow-up). Unlike St. Marks Hospital (53% – recommendations on time; 57% – patients with polyps receiving follow-up), the University of Utah Hospitals and Clinics also has a colonoscopy follow-up that is above the national and Utah averages (96% – recommendations on time; 95% – patients with polyps receiving follow-up). Emergency department (ED) care is a critical factor in enhancing patient recovery and complications. When comparing the three hospitals, St. Marks Hospital stands out as the best provider of ED care – it has the lowest wait time at the ED and no patients leave the ED before being seen by a physician (Medicare, 2020, a-c). Although Intermountain has a relatively good score when compared to the national average than the University of Utah Hospitals and Clinics, it needs to do more to improve ED wait time and ensure that patients do not leave the ED before they get professional assistance.
The success of a healthcare facility is intertwined with its ability to provide quality care relative to the cost incurred by the patients. Patients would want to feel that the care provided meets the amount of money they are spending – value for money. Medicare spending per beneficiary is highest at St. Marks Hospital and lowest at Intermountain Hospital – in all the three cases, it is slightly above the national and Utah averages (0.99 and 0.97 respectively). Across all the three healthcare facilities, the value of care is high and stable as depicted by the measurement metrics. Although there are some segments where the hospitals charge higher costs compared to industry averages, the outcomes are positive – no different or better than the national averages. From a cost perspective, University of Utah Hospital and Clinic has only one segment that exceeds the national average (payment for heart failure). St. Marks’ costs in heart failure, heart attack, and hip or knee replacements exceed the national average. On its part, Intermountain has costs that exceed the national average in hip or knee replacement and pneumonia treatment (Medicare, 2020, a-c). Overall, the scores show that there is a positive outlook in the value of care in the three hospitals.
Demographics and Services
Intermountain Hospital is the largest non-profit healthcare provider in Utah and serves the needs of all people in the region. The hospital provides a wide range of services, including acute care (Medicare, 2020, c). The Intermountain Hospital have five largest buildings; Carolyn Barnes Gardner Women and Newborn Center, J.L Sorenson Patient Tower, George and Dolores Outpatient Center, J. Sorenson Heart and Lung Center, and Jon and Karen Huntsman Cancer Center.
Intermountain targets both adults and children in need of medical care. Additionally, the hospital targets uninsured or low-income people, 14.9 percent of persons 65 years and over, about 14.8 percent of persons in poverty, 61.6 percent Whites, 17.6 percent Latino, 13.3 percent African American population. 1.2 percent American Indian, 5,6 percent Asian, and 0.2 percent Native Hawaiian (Pálsdóttir et al., 2016). Due to its size and history in the country, the healthcare facility has a multidimensional market approach – it does not target people based on income, age, race, religion, or nationality. The organization has developed a holistic approach of dealing with the needs of all people in the country; it does any discriminatory practices in the market. Through its community health programs, Intermountain conducts assessments to identify the areas that need healthcare interventions and develop implementation strategies to meet the needs of the people.
Intermountain Healthcare has implemented the patient’s responsibilities and rights for the protection of their patients. The hospitals prohibit patient discrimination of these roles and rights based on gender identity, sexual orientation, sex, socioeconomic status, mental ability, language, culture, religion, national origin, ethnicity, color, race, and age. At this hospital, patients are offered with remote sick people monitoring kit and other home-based health equipment’s. This equipment’s consist of the pulse oximeter, blood pressure monitor, digital scale, and cellular enabled digital
Intermountain Hospital is located in Murray in Utah on 0.40 km2. The hospital has over 75 regional branches spread in the country with a bed capacity of 452. It is located around UTA rail center near the parking lots. It has a number of services ranging from physician offices, research facilities, medical education, and cancer treatment hospital, newborn hospital, Level 1 trauma hospital, and a 15-story inpatient.
Cultural Dynamics
Modern medical institutions are providing care to culturally diverse populations (Tang et al., 2018). As explained by Lee et al. (2020), patients have a right to access culturally aligned and quality care from hospitals across the country. Besides, a culturally competent workforce enhances the experiences of the patients in a hospital environment. In lieu to the changing healthcare dynamics, culture is becoming a pivotal tool in evaluating the experience of patients in healthcare facilities. Culturally diverse care facilities can effectively address the unique needs of their patients than those that do not provide such services. It means that cultural dynamics can either increase or lower HCAHPS scores. If Intermountain adopts a culturally driven, quality care strategy, its HCAHPS scores will increase.
HCAHPS scores are widely used to assess patient’s perception on hospital treatment. HCAHPS are progressively crucial for hospitals and their quality presentation requirements. Cultural competence, therefore, improves the capacity of patients to communicate concerning their different realm of their life. Consequently, HCAHPS scores from health centers affect the cultural competency of hospitals on the basis of language, ethnicity, individual care and mixed case variables.
Educational Dynamics
Healthcare systems are complex and continuously changing within various service levels (Figueroa et al., 2019). Healthcare leaders need to respond to these changes by enhancing their capacities and improving the knowledge and skills of their workforce. As explained by Maier et al. (2018), nurses need to keep abreast of the changes through educational programs. Further, education is viewed as a tool to empower the patients to establish their independence in healthcare management. A highly educated workforce in a healthcare setting enhances the experience of the patients as it provides quality and reliable medical care services. Similarly, an educated or empowered community can bolster the experience of individual patients. Therefore, educational dynamics have an impact on the HCAHPS scores- presence of educational programs enhances the scores and absence of it lowers the scores, as the experiences of the patients are affected.
How Educational Dynamics Could Potentially Influence HCAHPS Scores
The educational dynamics can possibly affect HCAHPS scores. Patients are said to have different level of education and hence healthcare literacy. Patients with high low literacy skills and educational levels are said to hide their problems or inadequacies. They feel ashamed to accept their inability of reading and understanding healthcare information. This incidence is said to influence HCAHPS cores because of inability to understand the reading materials.
Socioeconomic Dynamics
The socioeconomic factors that affect healthcare include education, income, and employment (McMaughan et al., 2020). Access to quality and reliable care is a major factor that affects the experiences of patients. People who can access quality care are more likely to have positive experiences than those who cannot. Medical care accessibility is influenced by such factors as income and awareness on when to seek for such services. Hence, employed and educated individuals are more likely to access better care compared to unemployed and uneducated counterparts (Aloh et al., 2020). The accessibility to medical care influences the experiences of patients, and this translates to the changes in the HCAHPS scores. A positive socioeconomic indicator enhances the scores and a negative one lowers the scores.
Socioeconomic status privately affects HCAHPS scores. Those patients living in countries with ZIP Codes with lower averages typically rated healthcare better than those with higher salaries. Thus, cure of unknown number of patients with low incomes cannot be considered as pretex of unfair or poor HCAHPS scores.
Short-Term and Long-Term Financial Impact
Financial Impact
An increase in the flow of patients will translate to a positive financial performance. Considerably, the main role of financial management in hospitals is to manage finance and related risks as way of helping to realize the financial objectives of the healthcare. Increasing patients will increase cash flows in the hospital hence allowing it to meet daily operations. Similarly, the hospitals will also plan long tern financial projects such as construction due to increased cash flows.
Quality Outcomes
The success of any organization is influenced by its ability to meet the needs of the target customers. Like any other entity in the market, Intermountain needs to ensure that it enhances the experience of its patients. As explained by Al-Damen (2017), there is a strong relationship between patient experiences and quality of care. A positive patient experience is an indicator of quality and reliable care in a healthcare setting (Al-Damen, 2017). The HCAHPS scores recorded by Intermountain Medical Center indicate the provision of quality and reliable care in the community. By maintaining these scores, the hospital will increase its short and long-term financial performance.
Causes of the Hospital’s HCAHPS Scores
Intermountain Medical Center count on the fact that engaging patients in their personal care options results in improved clinical outcomes and highest possible satisfaction, both to the patient and the nurses. Crucial to these series of steps, if not actions, is transparency. Intermountain Medical Center offers impartial and non-partisan patient assessment report and feedback to assist people choose the hospital, rest assured that the they will receive the best possible services fit for their individual needs (Medicare, 2020, c). Additionally, causes of the hospital’s HCAHPS scores, are also as a result of the patient’s abilities to dispense sufficient feedback about their personal hospital experience, through the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The response rates and scores make it easier for people to weigh up different other hospitals alongside Intermountain Medical Center, and highlight supremacy, prowess and mastery in healthcare quality. Intermountain Medical Center’s five-star rating is an indication of the organization’s commitment and dedication to meet the needs of the patients. The healthcare organization has excelled when it comes to patient experiences, timeliness and effectiveness of care, management of complications and deaths, reduction of unplanned hospital visits, and effective use of medical imaging tests (Medicare, 2020, c).
The health systems put in place at Intermountain Medical Center allow for behavior change excursions to enhance patient engagement and scale people to quality healthcare. In other words, the hospital has optimized patient engagement, and focuses on getting the right people in moving in the right direction (Medicare, 2020, c). This entails getting loyal and accountable health workers to ensure quality health outcomes, without the need for rigorous direct engagement or intervention. By all means, Intermountain Medical Center endeavors to close gaps in care by bringing behavior change to the limelight of care delivery. This in so many dimensions, helps identify and mitigate high-risk, high-cost vulnerabilities along the care spectrum. This explains the hospital’s five-star rating as compared to other facilities.
Organizational Strategic Plan
Significance of Organizational Change
Organizational change empowers entities to confront problems and demands in their market – internal and external issues. Change is integral to the success of any business as it assists management to focus on issues that affect performance (Zarandi et al., 2017). Through organization change, Intermountain Medical Center can enhance the quality and reliability of its services. At the same time, organizational change will ensure that the healthcare organization will be in a position to address emerging issues in the community. For example, with organizational change strategies, Intermountain will be better positioned to handle the challenges bought about by the COVID-19 pandemic. As explained by Zarandi et al. (2017), organizational change is critical in addressing quality, leadership, employee engagement, technology, and financial issues – these factors influence the quality of care in a hospital setting. An improvement in the relevance of the services will lead to enhanced patient experiences, which will ultimately affect the HCAHPS scores. With the right leadership, technological tools, employees, and policies and regulations, Intermountain can enhance its patient experiences.
Intermountain needs to address some key areas to enhance or sustain its star ratings. Some of the areas within the national average that should be addressed include mortality, patient experience, effectiveness of care, and timeliness of care. While these areas are rated as some as the national averages, they need to be improved, if the hospital is to maintain its five-star ratings. However, no significant improvements will be attained without any changes in its operations, leadership, and policies and regulations. Hence, organizational change in the hospital will spearhead the provision of quality and reliable services that will address mortality, patient experiences, timeliness in care delivery, and effectiveness of care.
How Organizational Change Can Help Improve the Chosen Hospital’s HCAHPS Scores
The initial step is to affirm that there are effective organization resources and structures to reinforce efficient and fruitful enhancement initiatives. Organizations should also dedicate their human resources with service-oriented vacancies or positions to improve their chosen hospital’s HCAHPS scores. Additionally, organizations should also equip their workers with necessary skills for enhancing their patient experience in maintaining organization’s objectives. A team should also be designated to deal with patients as presented in HCAHPS facets that evaluate care, communication, and hospital setting. Organizations should improve HCAHPS scores via innovative ways of training their workers.
The Quality Strategic Framework
The quality strategic framework (QSF) will enhance the quality improvement priorities of Intermountain Medical Center. Intermountain strives to meet the needs of the patients in the community by actively engaging them and their families, committing to excellence based on experiences, and fostering a culture of quality improvement. The figure below shows the organization’s quality framework.
Figure 1.
Quality Strategic Framework
By providing quality care, Intermountain strives to enhance patient experience and improve its overall HCAHPS score. For the hospital to deliver the best patient experience, it must create a culture of continuous quality improvement, which will enable its workforce to identify, lead, and participate in quality improvement initiatives (Davidson et al., 2017). All the employees in the medical center must share clarity of purpose and support the organization’s goals. An academic focus will ensure that the hospital enhances the skills and knowledge of its workforce to provide great care to the patients. At the same time, quality improvement requires important changes in practices and processes in Intermountain. This is possible by looking at the status quo and adopting a coordinated approach to transition from processes that may hamper its performance. The figure below shows the QSF processes that will be integral in the success of Intermountain Medical Center.
Figure 2.
QSF Processes
The development of the QSF establishes a new approach of enhancing performance in Intermountain Medical Center. For the organization to succeed, it needs to have a vision that incorporates the expected changes, and supported by collaborative goals and objectives. The medical center’s vision is to enhance patient experience, by implementing such goals as education of its employees, implementation of technology, change in leadership, patient engagement, and continuous quality improvement. Continued support and communication among the stakeholders will guide the implementation of the action plans. Further, the creation of a strong quality improvement culture will be supported by progressive involvement of transformation leadership and sustainable quality improvement initiatives.
The strategic plan will lead to a patient-focused service delivery in the hospital. With quality improvement programs, it is expected that the healthcare facilities will improve its star ratings, particularly when it comes to patient experience. Furthermore, the plan will support and sustain system initiatives focused on quality. It will prioritize the integration of quality improvement in new activities and best patient experience will always be the target. Most importantly, the strategic plan will reduce the mortality rate, enhance effectiveness of care, and improve the provision of timely care in the hospital – areas that need urgent attention to enhance the medical center’s star ratings on patient experience.
Structure, Process, and Outcomes of the Strategic Plan
Structure is defined as the highest possible change which can be logically attributed to a program or an organization. The outcomes of strategic planning should, therefore, be designed with proper timeframe and one result established per every crucial area. Strategic process, on the other hand entails documentation and setting the direction of the organization. Strategic planning offers an organization with a clear values, vision, and mission.
Strategic planning at Intermountain Hospital should involve developing objectives and setting aims for where the hospital seeks to reach or achieve their vision. With these objectives and goals, the healthcare can design a practical plan for achieving their goals. These strategic plans are set in accordance with the financial trend, technological advancements, and government policies.
Strategic planning at Intermountain Hospital is crucial for its success. Grasping how this organizations works is crucial in creating practical strategic plan for the whole healthcare framework. This requires the management of the Intermountain Hospital to redesign the hierarchy on the company and decide the objective by establishing a clear path of achieving these goals. The management should, therefore, develop practical strategic plan for improving healthcare system of Intermountain Hospital.
In terms of the process, a far-reaching approach was applied to pinpoint the community health development strategies to address the associated and most common health priorities, which includes enhancing mental wellbeing, preventing avoidable illnesses and unintended accidents and improving air quality throughout the Intermountain health system in each hospital’s strategic plan.
Noteworthy, establishing Criteria for Community Health Improvement Strategies Intermountain presented the CHNA results to local stakeholders, many of whom were later identified as collaborative partners in each hospital community and worked hand in hand with the hospital management to generate a comprehensive directory of the current community programs and involvements to address the identified health precedence through community input meetings (Intermountain Utah Valley Hospital, 2020). Additionally, Intermountain’s community health implementation planning team performed a checklist of all Intermountain Medical Center programs and initiatives to identify those evidence-based best practices with application to community health improvement initiatives. The community health implementation planning team scored and vetted both internal and externally proposed strategies and conducted a thorough literature review on evidenced-based programs that addressed the health priorities and demonstrated health improvement.
The inventory of evidence-based interventions was scored by the Intermountain community health implementation planning team according to the following dimensions: ability to implement and maintain fidelity to achieve anticipated outcomes, cost – total expense of the intervention (education materials, instructor, screening supplies, promotional materials, evaluation and data management), and effectiveness – measure of improved health as a result of intervention (Intermountain Utah Valley Hospital, 2020).
Incorporation of Evidence-Based Practice (EBP) and Shared Governance
Evidence-based practice (EBP) is integral in the provision of patient-centered care (PCC). As explained by Lehane et al. (2018), it centers on using the available patient information to recommend medical interventions. The promotion of EBP requires organizations to have reliable infrastructure committed to supporting its delivery. The incorporation of EBP in Intermountain will start by developing supporting infrastructure, including technologies to support data collection, storage, and analysis. The second step is the development of EBP driven goals and objectives – PCC goals. With a clear vision and targets in place, the employees will be educated on the use of EBP. Finally, progressive developments will be made to use new and emerging technologies to support healthcare decisions.
Shared governance is the structure and process for accountability, partnership, and ownership. It ensures that individuals are responsible for their decisions in a work environment. The incorporation of shared governance in Intermountain starts by developing laws detailing the structure of leadership. With a redefined governance structures, leaders and employees are tasked with specific responsibilities. Further, delegation of duties will be prioritized to ensure that low-ranking employees have decision-making responsibilities. The role of leaders in the organization will include coaching and mentoring to pave the way for creativity and productivity among the employees. Acting as developmental facilitators, leaders in Intermountain will allow teams to function smoothly. At the same time, shared governance will be attained by having an open communication structure. Free flow of information will facilitate communication and reduce the bottlenecks that hamper decision-making.
Shared Accountability
Shared accountability involves everyone, including patients, insurers, physicians, and the community in the provision of medical care. The development of shared accountability in Intermountain takes into perspective redesign care using the available standards, engaging patients, and aligning financial incentives in care provision for all stakeholders. Medical providers are expected to engage patients on the best care plans. They should run diagnostics, prescribe appropriate medications, and follow-up on EBP driven care. Physicians and other medical care providers should be involved in held accountable by involving them in planning and tracking their activities. Payers need to be held accountable by monitoring their financing activities by adopting a feedback loop that encourages timely reimbursements. Employees in the organization will be held accountable through frequent assessment of their performance by their departments. As explained by James (2019), monitoring progress, developing accountability conversations, and having a culture of accountability will be integral in building shared accountability at Intermountain Medical Center. The overarching element in developing shared accountability is the incorporation of technology in the management process. Through technological tools, management can monitor the activities of all stakeholders involved in care provision, particularly the internal stakeholders.
Incorporation of Technology
Technology has become ubiquitous in almost every sphere of the society. Through technology, businesses can enhance the relevance and effectiveness of their services. As explained by Bove (2019), digital technology enhances the interaction between healthcare facilities and patients. The use of technology in Intermountain Medical Center can foster its star ratings by enhancing the experiences of the patients. Technology can enhance healthcare practitioners to diagnose issues quickly and prevent readmissions. Two strategies can be used to incorporate technology trends in within Intermountain Medical Center: in-house development and outsourcing. The in-house development method is vital to the adoption of specific technologies that will drive sensitive activities in the healthcare facilities. Moreover, this method is vital to the adoption of unavailable technologies in the market. An outsourcing methodology is crucial when cutting costs and saving time. The combination of the two methods will ensure that Intermountain has the best technologies to deal with emerging issues in the market.
Technology Trends
Healthcare industry is rapidly evolving and hence the need for using modern technologies in transforming health services in hospitals. Some of the methods which can be used in the digital healthcare are nanotechnology, robotics, 3D-printing, VR/AR, and artificial intelligence. The healthcare sector is currently familiarizing with the current developments to control technology. The healthcare sector is presently depending on latest technology and hence the healthcare workers have to adopt emerging healthcare technologies to remain relevant in future.
Improving Care Delivery System
The concept of quality improvement requires change. However, without a clear plan, change often fails. Thus, improving Intermountain Medical Center’s care delivery system requires effective planning and leadership. The first step in addressing the hospital’s care delivery system is to develop policies and regulations that will set the minimum quality standards and procedures in managing patient needs. The approach takes into consideration the industry’s standards on quality. In this case, quality relates to the satisfaction of the needs of the patients. Performance benchmarking is the ideal method of managing quality in the medical center. The method uses industry standards and targets as thresholds in enhancing organizational performance. Using the method, the hospital strives to exceed the national or state averages.
Improving care delivery in Intermountain requires the management of costs. The ideal method that the organization can use is cost budgeting, which involves estimating costs of resources and allocating them to cost accounts. It means that performance is measured against the incurred costs. At the same time, industry standards will offer guidance on critical areas and the average costs expected to be incurred. By managing costs, the organization can optimize performance and enhance productivity. The long-term aim is to ensure that the hospital lowers its operating costs and maximizes patient satisfaction.
Medical care accessibility is another area that must be addressed to enhance care delivery in Intermountain. This area can be enhanced through the integration of technology in the healthcare organization. The adoption of patient-monitoring systems and off-site treatment options will lower the cost of medical care and enhance the interaction between patients and healthcare providers. Such technologies as telemedicine are vital to the success of the hospital, especially as a non-profit agency. Moreover, the adoption of technology facilitates the provision of patient-centered care (PCC). The use of wearable technologies will allow nurses to collect and analyze patient data that will be vital in assessing the needs of their patients. The incorporation of big data in the hospital will support the use of PCC approach.
Methods of Improving the Care Delivery System
Increasing healthcare costs, higher number of insured patients, and increased understanding of medical mistakes helps in improving care delivery system. Presently, efforts on patient safety and outcomes, cost cutting, efficiency, care coordination and care redesign are assessed to control quality of healthcare. Ultimately, to control care delivery system an effective team should consist of staff from different cultural backgrounds as well as vast experience and skills levels.
Improve Financial Stability
Intermountain Medical Center does not have a specific customer segment – it targets all patients in the community. While this is a good approach of maintaining its reputation as a non-profit agency, the organization needs to develop a marketing segmentation approach. The classification of the patients will ensure Intermountain develops strategies to meet the specific needs of a group of patients with similar interests. At the same time, it is a viable option of expanding its customer base and take advantage of economies of scale. Further, the hospital needs to enhance its customer conversation rate – build customer loyalty. By enhancing patient experiences, Intermountain can have a large pool of loyal customers who will consequently enhance its financial stability. Apart from the revenue generation abilities, Intermountain needs to focus on cost management (Samorodov et al., 2019).
Methods That Would Be Used to Improve Financial Stability
Instead of purchasing costly equipment, management can consider to lease, especially if they are not to be used for long periods. Reduction of overhead costs by adopting digital strategies and green sources of energy will offer the organization an opportunity to lower its operating costs.
Implementation Plan and Timeline
Roles and Responsibilities of Stakeholders
The stakeholders involved in the development and implementation of the strategic plan include the support staff, nursing staff, doctors, nursing leaders, administrators, regulatory agencies, and the board of directors. The role of the support staff is to identify the loopholes in the hospital that impair its performance. The support staff will provide critical information and directions on such issues as overhead costs, security, hygiene, and other issues that affect the daily routines of the hospital. The nursing staff and doctors provide crucial guidelines on dealing with patients and evaluation of their experiences. They determine the right treatment protocols and the guidelines to incorporate PCC. Administrators organize the daily routines of the hospital, including admission of patients. They are responsible for ensuring that change takes place in the hospital. Moreover, they mobilize resources to be used in enhancing change. Regulatory agencies authorize the recommended strategies to ensure that they do not violate existing laws and standards. The nursing leaders organize and mobile the nursing staff to accept and facilitate change. The board of directors approves short-term and long-term goals that may spur organizational change. They authorize the new vision and recommended strategies to enhance organizational performance.
Key Roles and Responsibilities of Stakeholders
Stakeholder Accountability and Involvement
Accountability is improved by delegating duties and setting SMART goals for the all the stakeholders. Each stakeholder’s performance is then evaluated to measure their progress and make any changes to improve their outcomes. An outcome-based approach of monitoring the work of the stakeholders will ensure that they remain accountable for their actions. Further, setting realistic timelines will ensure that stakeholders remain accountable for their roles and responsibilities. Another conventional approach to enhance accountability is to ensure that team members express their commitment either verbally or in writing to assist in the implementation of the strategic plan.
A project cannot succeed without the involvement of stakeholders (Daniel & Inim, 2020). For Intermountain Medical Center’s stakeholders to have an impact on its performance, they need to be involved in the implementation of the strategic plan. Thus, their engagement will commence early to identify their needs and expectations. The development of the goals, objectives, and timelines will involve the stakeholders. The adoption of an open communication system will ensure that stakeholders share their views on the relevance of the strategic plan and its implementation. Further, the creation of diverse teams will give stakeholders an opportunity to participate in the success of the business.
How to Ensure Stakeholder Accountability And Involvement
One way to ensure stakeholder accountability and involvement is through evaluation. This method ensures stakeholders learn and that they are accountable for their performance and involvement in organization. Evaluation also ensures that stakeholders give an account of their performance. Evaluation, however, can be underpinned through learning. Additionally, stakeholder accountability and involvement can be ensured through commitment. The latter, therefore, can be realized through responsiveness and responsiveness.
Staff Training
Staff training is crucial in increasing their awareness and reducing the knowledge and skill gap in a healthcare setting (Arain et al., 2019). As Intermountain seeks to transition towards a digitized enabled service delivery model, it is pertinent for the staff to be trained. Acquisition of technological skills will ensure that the staff effectively uses big data and the internet of things technologies to provide patient-centered care. They will also need to train on addressing diversity issues, including culture and religion. The ability to meet the needs of varying groups in the community will ensure that patient experience is enhanced. At the same time, training on working in multidisciplinary teams will ensure that the staff fosters the interprofessional collaboration for the sake of the patients.
How to Train Staff
Employee training is crucial in several ways. First, it significantly assists in improving worker engagement and increase employee retention. Second employee training increases the productivity and efficiency of an organization. For this reason, there is need for establishing proper worker training which is effective. A training approach should be developed to realize educational objectives in an organization. Developing training techniques entails preparing workers with high-tech skills needed in executing complex tasks in an organization. Employees should also be trained regularly to ensure they remain competitive in their roles.
Methods of Training Staff
Plan Timeline
Table 5.
Plan timeline in months
| Description | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| Requirement gatherings | |||||||||
| Develop vision, goals and objectives | |||||||||
| Develop and disseminate plan to stakeholders | |||||||||
| Align processes with new plan and conduct evaluations to make any changes | |||||||||
| Training and deployment of the new plan | |||||||||
| Implementation of the plan with new changes | |||||||||
| Evaluation |
As illustrated in the table above, the plan is expected to take 9 months to be implemented. Evaluations of the plan are conducted on a monthly basis, as it allows management to track any changes in all the phases. Performance measurements (comparing period before and after the new plan) are vital to track the impact of the new plan and monitor the progress of the hospital in adopting new changes.
Evaluation of the Strategic Plan
An outcome-based method is used to evaluate the success of the strategic plan. The aim of the plan is to enhance Intermountain Medical Center’s star rating by enhance patient experiences. By conducting an outcome-based evaluation, the broader impacts of the strategic plan will be investigated. The comparison of the period prior and after the adoption of the strategic plan will aid in understanding any progress attained. The evaluations will be conducted on a monthly basis – an ideal timeline to assess the provision of quality care that improves patients’ experiences. Through surveys, the hospital can determine the experiences of the patients due to the new changes. The applicable method of analysis is descriptive statistics. The choice of the method is informed by the desire to evaluate the prevalence of common experiences among the patients. Descriptive analysis offers an opportunity for management to cluster common experiences and either work to enhance or sustain the operations of the hospital.
To evaluate the success of the strategic plan, there are number of aspects which will be considered. First, a checklist will be established that would be used to assess the objectives of the organization. A few emails will be sending to customers to evaluate their feedback about the products or services they received from the organization. The capacity of the organization to expand or growth will also be analyzed in order to ascertain the success of the strategic plan.
Stakeholder Involvement
The stakeholders will be part of the evaluation teams to ensure their involvement in assessing the impact of the strategic plan. Continued involvement of the stakeholder through select teams will ensure that their feedback is adopted. Further, feedback will be shared with the stakeholders during every evaluation period. Engaging or involving stakeholders during evaluation implementation and planning increases value by offering perceptions of what is considered useful evaluation, high quality, and credible evaluation. Stakeholders will take part in helping designing evaluation tools. They will be part of the group or team that will analyze data. Stakeholders will also be part of organizations internal assessment team.
Communication of Evaluation Results
Communication is facilitated through internal and external channels. The internal channels include the company’s intranet system, memos and website. The external communication platforms include e-mails and social media groups. The sharing of information through these communication channels will ensure that all stakeholders are informed. Sensitive information will not be shared on the external communication platforms but will be limited to the internal communication channels and shared among select individuals. Further, periodic meetings will be organized to update primary stakeholders on the outcome of the plan.
References
Al-Damen, R. (2017). Health care service quality and its impact on patient satisfaction “Case of Al-Bashir hospital”. International Journal of Business and Management, 12(9), 136. https://doi.org/10.5539/ijbm.v12n9p136
Aloh, H. E., Onwujekwe, O. E., Aloh, O. G., Okoronkwo, I. L., & Nweke, C. J. (2020). Impact of socioeconomic status on patient experience on quality of care for ambulatory healthcare services in tertiary hospitals in southeast Nigeria. https://doi.org/10.21203/rs.2.19043/v3
Arain, M. A., Tarraf, R., & Ahmad, A. (2019). Assessing staff awareness and effectiveness of educational training on IT security and privacy in a large healthcare organization. Journal of Multidisciplinary Healthcare, 12, 73-81. https://doi.org/10.2147/jmdh.s183275
Bove, L. A. (2019). Increasing patient engagement through the use of wearable technology. The Journal for Nurse Practitioners, 15(8), 535-539. https://doi.org/10.1016/j.nurpra.2019.03.018
Cox, C., & Amin, K. (2020, August 10). How have healthcare utilization and spending changed so far during the coronavirus pandemic? Peterson-KFF Health System Tracker. https://www.healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/#item-start
Daniel, C. O., & Inim, V. (2020). Role of project managers in the stakeholder management. International Journal of Scientific and Research Publications (IJSRP), 10(1), p9741. https://doi.org/10.29322/ijsrp.10.01.2020.p9741
Davidson, K. W., Shaffer, J., Ye, S., Falzon, L., Emeruwa, I. O., Sundquist, K., Inneh, I. A., Mascitelli, S. L., Manzano, W. M., Vawdrey, D. K., & Ting, H. H. (2017). Interventions to improve hospital patient satisfaction with healthcare providers and systems: A systematic review. BMJ Quality & Safety, 26(7), 596-606. https://doi.org/10.1136/bmjqs-2015-004758
Figueroa, C. A., Harrison, R., Chauhan, A., & Meyer, L. (2019). Priorities and challenges for health leadership and workforce management globally: A rapid review. BMC Health Services Research, 19(1). https://doi.org/10.1186/s12913-019-4080-7
Grustam, A., Jovic Vranes, A., Soldatovic, I., Stojicic, P., & Jovanovic Andersen, Z. (2020). Factors associated with utilization of primary and specialist healthcare services by elderly cardiovascular patients in the Republic of Serbia: A cross-sectional study from the national health survey 2013. International Journal of Environmental Research and Public Health, 17(7), 2602. https://doi.org/10.3390/ijerph17072602
Intermountain Utah Valley Hospital. (2020). Utah Valley Hospital implementation strategy plan 2020-2021. https://intermountainhealthcare.org/ utah-valley-hospital-implementation-strategy-plan 2020-2021
Intermountain Healthcare. (2021). About Intermountain. intermountainhealthcare.org. https://intermountainhealthcare.org/about/who-we-are/mission-vision-values/
James, T. A. (2019). How leaders create a culture of accountability in health care. Lean Forward. https://leanforward.hms.harvard.edu/2019/08/15/how-leaders-create-a-culture-of-accountability-in-health-care/
Lee, S. E., Lee, M. H., Peters, A. B., & Gwon, S. H. (2020). Assessment of patient safety and cultural competencies among senior baccalaureate nursing students. International Journal of Environmental Research and Public Health, 17(12), 4225. https://doi.org/10.3390/ijerph17124225
Lehane, E., Leahy-Warren, P., O’Riordan, C., Savage, E., Drennan, J., O’Tuathaigh, C., O’Connor, M., Corrigan, M., Burke, F., Hayes, M., Lynch, H., Sahm, L., Heffernan, E., O’Keeffe, E., Blake, C., Horgan, F., & Hegarty, J. (2018). Evidence-based practice education for healthcare professions: An expert view. BMJ Evidence-Based Medicine, 24(3), 103-108. https://doi.org/10.1136/bmjebm-2018-111019
Maier, C. B., Budde, H., & Buchan, J. (2018). Nurses in expanded roles to strengthen community-based health promotion and chronic care: Policy implications from an international perspective; a commentary. Israel Journal of Health Policy Research, 7(1). https://doi.org/10.1186/s13584-018-0257-5
McMaughan, D. J., Oloruntoba, O., & Smith, M. L. (2020). Socioeconomic status and access to healthcare: Interrelated drivers for healthy aging. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.00231
Medicare. (2020, a). University of Utah Hospitals and Clinics. Medicare.gov: the official U.S. government site for Medicare | Medicare. https://www.medicare.gov/care-compare/details/hospital/460009?id=ae230381-8594-44ec-ab1b-ae801610b931&city=Salt%20Lake%20Cty&state=UT#ProviderDetailsRatingsContainer
Medicare. (2020, b). St Mark’s Hospital. Medicare.gov: the official U.S. government site for Medicare | Medicare. https://www.medicare.gov/care-compare/details/hospital/460047?id=0095abc9-9c78-4a45-9743-5530bb375349&city=Slc&state=UT
Medicare. (2020, c). Intermountain Medical Center. Medicare.gov: the official U.S. government site for Medicare | Medicare. https://www.medicare.gov/care-compare/details/hospital/460010?id=d5d9491e-7f88-4e37-a0d3-f3b6a8af240f&city=Salt%20Lake%20City&state=UT
Medicare. (2020, c). (Images). Medicare.gov: the official U.S. government site for Medicare | Medicare. https://www.medicare.gov/care-compare/details/hospital/460010?id=d5d9491e-7f88-4e37-a0d3-f3b6a8af240f&city=Salt%20Lake%20City&state=UT
Pálsdóttir, B., Barry, J., Bruno, A., Barr, H., Clithero, A., Cobb, N., … & Worley, P. (2016). Training for impact: the socio-economic impact of a fit for purpose health workforce on communities. Human Resources for Health, 14(1), 1-9.
Samorodov, B., Azarenkova, G., Golovko, O., Oryekhova, K., & Babenko, M. (2019). Financial stability management in banks: Strategy maps. Banks and Bank Systems, 14(4), 10-21. https://doi.org/10.21511/bbs.14(4).2019.02
Tang, C., Tian, B., Zhang, X., Zhang, K., Xiao, X., Simoni, J. M., & Wang, H. (2018). The influence of cultural competence of nurses on patient satisfaction and the mediating effect of patient trust. Journal of Advanced Nursing, 75(4), 749-759. https://doi.org/10.1111/jan.13854
Zarandi, H. M., Amirkabiri, A., & Azimi, H. (2017). The role of organizational change on improving organizations financial and economic performance (Case study: Bank Shahr). A Quarterly Journal of Urban Economics and Management, 5(18), 117-130.